The anti-vaccination movement: an ally of the COVID-19
DOI:
https://doi.org/10.46661/revintpensampolit.5598Keywords:
Anti-vaccines, COVID-19, vaccines, research, pandemicsAbstract
The development of an effective vaccine that protects against the new coronavirus is expected to be the key to overcome the current pandemics. If the vaccine is administered to a majority of the people, this protection could eventually become global. Nevertheless, the growing anti-vaccine movement may hinder the herd effect and lengthen the virus persistence among the population. The present work argues in favor of a necessary debate on vaccination refusal, unavoidable within the framework of health emergency due to the SARS-CoV-2 pandemics.
Downloads
References
Abbott, A. (2020). Researchers highlight ‘questionable’ data in Russian coronavirus vaccine trial results. Nature, 585(7826), 493-493. https://doi.org/10.1038/d41586-020-02619-4
Aguas, R., Corder, R. M., King, J. G., Gonçalves, G., Ferreira, M. U., & Gabriela Gomes, M. M. (2020). Herd immunity thresholds for SARS-CoV-2 estimated from 1 unfolding epidemics. medRxiv, 2020.07.23.20160762. https://doi.org/10.1101/2020.07.23.20160762
ASSET. (2017). Compulsory vaccination and rates of coverage immunistion in Europe, 1–6. http://www.asset-scienceinsociety.eu/reports/page1.html
Ball, P. (2020). Anti-vaccine movement could undermine efforts to end coronavirus pandemic, researchers warn. Nature, 581(7808), 251.
Benecke, O., & DeYoung, S. E. (2019). AntiVaccine Decision-Making and Measles Resurgence in the United States. Global Pediatric Health, 6, 2333794X1986294. https://doi.org/10.1177/2333794x19862949
Britton, T., Ball, F., & Trapman, P. (2020). A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2. Science, 369(6505), 846-849. https://doi.org/10.1126/science.abc6810
Burki, T. (2020). The online anti-vaccine movement in the age of COVID-19. The Lancet Digital Health, 2(10), e504e505. https://doi.org/10.1016/s2589-7500(20)30227-2
Chen, W. H., Strych, U., Hotez, P. J., & Bottazzi, M. E. (2020). The SARS-CoV-2 Vaccine Pipeline: an Overview. Current Tropical Medicine Reports, 7(2), 61-64. https://doi.org/10.1007/s40475-020-00201-6
Comité Asesor de Vacunas de la AEP. (2018, octubre). Capítulo 44. Manual de vacunas en línea de la Asociación Española de Pediatría (AEP).https://vacunasaep.org/profesionales/noticias/manual-de-vacunas-en-linea-actualizacion-octubre-2018
Donvan, J., & Zucker, C. (2017). Outra Sintonia. A História do Autismo. Companhia Das Letras.
Ehreth, J. (2003). The global value of vaccination. Vaccine, 21(7-8), 596-600. https://doi.org/10.1016/S0264-410X(02)00623-0
GALLUP. (2019). Wellcome Global Monitor-First Wave Findings. 1-132. https://wellcome.org/sites/default/files/wellcome-global-monitor-2018.pdf
Grupo ENE-COVID. (2020). Estudio ENE-COVID: Informe final estudio nacional de sero-epidemiología de la infección por Sars-CoV-2 en España (1–32).
Instituto de Salud Carlos III. (2020, julio). Monitorización del comportamiento y las actitudes de la población relacionadas con el COVID-19 en España (COSMO SPAIN): Estudio OMS. COSMO-SPAIN.
Jackson, L. A., Anderson, E. J., Rouphael, N. G., Roberts, et al. (2020). An mRNA Vaccine against SARS-CoV-2 — Preliminary Report. New England Journal of Medicine. https://doi.org/10.1056/nejmoa2022483
Khan, Y. H., Mallhi, T. H., Alotaibi, N. H., Alzarea, A. I., Alanazi, A. S., Tanveer, N., & Hashmi, F. K. (2020). Threat of COVID-19 vaccine hesitancy in Pakistan: The need for measures to neutralize misleading narratives. American Journal of Tropical Medicine and Hygiene, 103(2), 603-604. https://doi.org/10.4269/ajtmh.20-0654
Lurie, N., Saville, M., Hatchett, R., & Halton, J. (2020). Developing Covid-19 Vaccines at Pandemic Speed. New England Journal of Medicine, 382(21), 1969-1973. https://doi.org/10.1056/NEJMp2005630
Miembros del Comité de Bioética de España. (2016). Cuestiones ético-legales del rechazo a las vacunas y propuestas para un debate necesario. http://assets.comitedebioetica.es/files/documentacion/es/cuestiones-etico-legales-rechazo-vacunas-propuestas-debate-necesario.pdf
Motta, M., Callaghan, T., & Sylvester, S. (2018). Knowing less but presuming more: Dunning-Kruger effects and the endorsement of anti-vaccine policy attitudes. Social Science and Medicine, 211, 274-281. https://doi.org/10.1016/j.socscimed.2018.06.032
Offit, P. A. (2005). The cutter incident, 50 years later. New England Journal of Medicine, 352(14), 1411-1412. https://doi.org/10.1056/NEJMp048180
Offit, P. A., & Salisbury, D. M. (2012). Should childhood vaccination be mandatory? Yes/No. BMJ (Online), 344(7858). https://doi.org/10.1136/bmj.e2435
Olive, J. K., Hotez, P. J., Damania, A., & Nolan, M. S. (2018). The state of the antivaccine movement in the United States: A focused examination of nonmedical exemptions in states and counties. PLOS Medicine, 15(6), e1002578. https://doi.org/10.1371/journal.pmed.1002578
Ploomipuu, I., Holbrook, J., & Rannikmäe, M. (2019). Modelling health literacy on conceptualizations of scientific literacy. Health Promotion International. https://doi.org/10.1093/heapro/daz106
Rochel de Camargo, K. (2020). Here we go again: the reemergence of anti-vaccine activism on the Internet. Cadernos de saude publica, 36 2, e00037620. https://doi.org/10.1590/0102-311x00037620
Rutjens, B. T., Sutton, R. M., & van der Lee, R. (2018). Not All Skepticism Is Equal: Exploring the Ideological Antecedents of Science Acceptance and Rejection. Personality and Social Psychology Bulletin, 44(3), 384-405. https://doi.org/10.1177/0146167217741314
Valera, L., Vergara, P. R., Barreaux, I. P., & García, P. B. (2019). Parental refusal to mandatory vaccination in Chile. Ethical and legal challenges. Revista Chilena de Pediatria, 90(6), 675-682. https://doi.org/10.32641/rchped.v90i6.1002
Vaz, O. M., Ellingson, M. K., Weiss, P., Jenness, S. M., Bardají, A., Bednarczyk, R. A., & Omer, S. B. (2020). Mandatory vaccination in Europe. Pediatrics, 145(2). https://doi.org/10.1542/peds.2019-0620
Wakefield, A. J., Murch, S. H., Anthony, A., Linnell, J., Casson, D. M., Malik, M., Berelowitz, M., Dhillon, A. P., Thomson, M. A., Harvey, P., Valentine, A., Davies, S. E., & Walker-Smith, J. A. (1998). RETracted: Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet, 351(9103), 637-641. https://doi.org/10.1016/S0140-6736(97)11096-0
Wang, J., Peng, Y., Xu, H., Cui, Z., & Williams, R. O. (2020). The COVID-19 Vaccine Race: Challenges and Opportunities in Vaccine Formulation. AAPS PharmSciTech, 21(6). https://doi.org/10.1208/s12249-020-01744-7
Warren, M. (2019). Vaccination rates rise in Italy and France after law change. Nature. https://doi.org/10.1038/d41586-019-02193-4
WHO. (2008). Vaccination greatly reduces disease, disability, death and inequity worldwide. Bulletin of the World Health Organization, 86(2).
World Health Organization. (2020). Draft landscape of COVID-19 candidate vaccines. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines
Wong, C. H., Siah, K. W., & Lo, A. W. (2019). Estimation of clinical trial success rates and related parameters. Biostatistics, 20(2), 273-286. https://doi.org/10.1093/biostatistics/kxx069
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Open access policy
Free and open access is allowed to any interested party to all the contents of the journal issues, free of charge, being able to print and transfer all the articles, with the only condition of specifying the source and authorship.
The journal: a) does not charge authorship costs for the processing of articles or for their submission, b) maintains copyright for authors without restrictions, c) facilitates authors to keep their publication rights without limitations.
The International Journal of Political Thought is an original work of the Laboratory of Political Ideas and Practices of the Pablo de Olavide University. All articles included in the Journal are original work of their respective authors. This Journal is freely offered to the scientific and academic community at no cost and releases the contents according to the license "Attribution-NonCommercial-ShareAlike 4.0 CC BY-NC-SA" of the Creative Commons project available in the following url: https://creativecommons.org/licenses/by-nc-sa/4.0/legalcode
If you wish to translate or compile any of the articles available here, please contact us at contacto







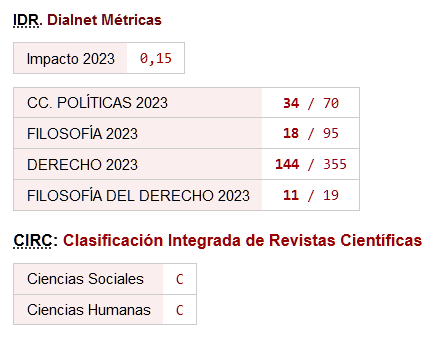



 ISSN: 1885-589X
ISSN: 1885-589X  Universidad Pablo de Olavide
Universidad Pablo de Olavide